Sleep Apnea Guide
Sleep Apnea
Millions of Americans have a sleep disorder. Insomnia is most commonly known, yet sleep apnea is prevalent, but not as well known and often undiagnosed. However, the signs and symptoms are conspicuous.
Do you snore? Do you have type 2 diabetes or prediabetic? Are you overweight or obese? Such symptoms or overlapping conditions are related to obstructive sleep apnea (OSA). For example, sleep apnea affects 3 percent of those who are overweight and over 20 percent of those who are obese.1
Actually, sleep apnea affects the body from head to toe. It’s important to understand what it is so you can recognize symptoms and seek proper treatment. Living with an undiagnosed case of OSA disrupts the body and mind – it can even be fatal.
What Is Sleep Apnea?
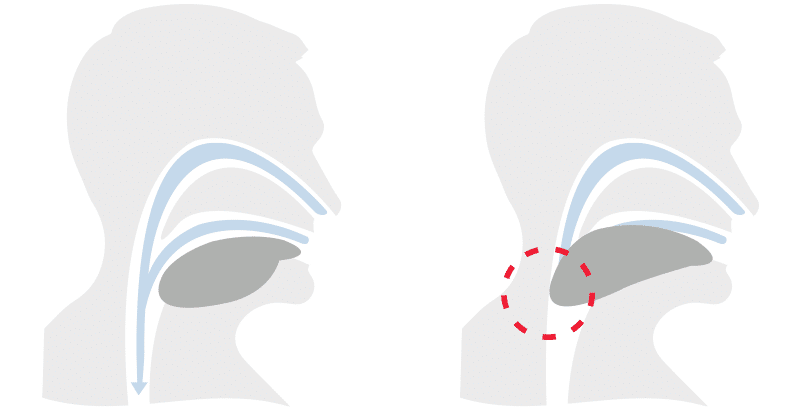
Snoring is a hallmark trait of sleep apnea.2 Those with obstructive sleep apnea suffer from a completely or partially blocked airway. The absolute blockages are called apneas. Hypopneas are partial blockages. Both decrease airflow and oxygen saturation, limiting the amount of oxygen getting to red blood cells and often induce snoring.3 Apneas and hypopneas are both associated with sleep apnea, and individuals with the sleep disorder may experience both.
To date, sleep clinicians recognize three types of sleep apnea: obstructive, central, and complex. While obstructive sleep apnea is due to complete or partial blockages of air, central sleep apnea involves no physical obstruction. It’s caused by a miscommunication between throat muscles and the brain.
Making the sleep disorder more complex, doctors discovered some sleep apnea patients suffer from both types which is often referred to as mixed sleep apnea (otherwise known as complex sleep apnea).
How Many People Suffer From Sleep Apnea?
New research presented at the annual meeting of the Associated Professional Sleep Societies in 2019 estimates 170 million adults have obstructive sleep apnea (OSA). This estimate is based on a large scale analysis of obstructive sleep apnea (OSA) prevalence in the Americas (North, Central, and South America). Of the 40 countries, the U.S. is identified as the country with the greatest number of estimated adults with OSA with 54 million.4
The actual number of diagnosed obstructive sleep apnea patients in the US is much lower. A Frost and Sullivan report commissioned by the American Academy of Sleep Medicine reported 5.9 million U.S. adults are diagnosed with OSA, with and estimated 23.5 million U.S. adults remaining undiagnosed.5 This estimation is based on a 2013 study published in PubMed, based on data from the landmark Wisconsin Sleep Cohort Study (1988-1994 and 2007-2010).6
The American Sleep Apnea Association reports on their website that approximately 22 million Americans suffer from sleep apnea. So why is there such a huge discrepancy in the estimated number of people who have obstructive sleep apnea? The question of how many people have obstructive sleep apnea (OSA) may seem fairly straightforward, but answering it accurately and with absolute certainty is not.
There are few large scale studies and the sleep disorder is largely underreported and undiagnosed. The underreporting and underdiagnosis is in part due to a lack of education (among healthcare practitioners and laypeople), in addition to an underappreciation of the seriousness of the condition.
Although the recent 2019 statistic indicating 54 million U.S.adults have OSA (with the vast majority living unknowingly with the sleep disorder) isn’t as widely known or cited yet, it is accepted as a more accurate estimation of cases by sleep professionals in the field.
Even more concerning than the total estimation of OSA cases, is the estimated number of people suffering from moderate to severe sleep apnea which comes with serious health risks such as stroke, hypertension and diabetes. It’s estimated that of the 170 million adults cited in the study, that 81 million falls in this moderate to severe range.
Can You Get Sleep Apnea at Any Age??
Sleep apnea can occur at any age; however, it’s more common in people over the age of 40. Studies from the American Thoracic Society (ATS) show the prevalence of sleep apnea increases as a person ages. Adult men from various ages were studied, and the results are as follows – sleep apnea has a prevalence of:
- 3.2% in men between the ages of 20-44 years old
- 11.3% in men between the ages of 45-64 years old
- 18.1% in men between the ages of 61-100 years old
One reason why the prevalence percentage increases with age is that older populations usually have more fatty deposits in the neck area.
Types of Sleep Apnea
Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) is the most common type of sleep apnea. It’s categorized by sporadic breaks in breathing or partial obstructions, upwards of five or more times per hour, as muscles in the back of the throat fail to stay open and/or fatty tissue blocks the flow of air. An obstruction to breathing sounds quite troubling, yet it’s very treatable with CPAP therapy.7
Clinicians diagnose OSA in terms of mild to severe depending on the number of times the apneas occur throughout the night. 80% of moderate to severe cases go untreated, but untreated cases don’t result in snoring alone.8 A host of associated health risks can develop for those living with untreated OSA, including diabetes, hypertension, and heart disease.
Central Sleep Apnea
Central sleep apnea is caused by a miscommunication between throat muscles and the brain, and is rare compared to obstructive sleep apnea. This form of sleep apnea is caused when the brain ”forgets” to instruct the muscles to breathe, which creates apneas. A sleeper does not stop breathing, because the respiratory effort stays intact, yet the sleeper misses breaths.
Central sleep apnea may occur due to other conditions, such as heart failure, stroke, or sleeping at higher altitudes.9 While historically rare, cases of central sleep apnea are rising due to the recent abuse of opioids and prescription medicine.10
Since there is no obstruction, snoring may not be a symptom of central sleep apnea. However, seek treatment if you experience episodes of paused or abnormal breathing while sleeping or abrupt awakenings followed by a shortness of breath.
Complex Sleep Apnea
In 2006, Mayo Clinic sleep clinicians encountered a rare phenomenon when treating patients with OSA.11 Despite receiving CPAP (continuous positive airway pressure), which unblocks airways, some patients were not breathing as they should. Some of those initially assumed to be suffering from only OSA, were actually showing symptoms of central sleep apnea when given CPAP treatment.
Snoring, anxiety, and poor concentration are just some of the more common symptoms related to sleep apnea. As you’ll learn, symptoms may overlap with other conditions and occur day and/or night, making it crucial to better understand the symptoms and risks associated with untreated sleep apnea.
Sleep Apnea Symptoms
Have you been told that you snore? As mentioned, that’s a signal of sleep apnea. But, that’s not likely the worst of your problems if you’re living with undiagnosed obstructive sleep apnea. The sleep disorder is linked to inconvenient symptoms such as snoring and daytime sleepiness, but compounded over time, symptoms grow more dire, even life threatening.12
What’s additionally concerning is those suffering from sleep disorders may believe it’s due to some other reason or overlapping condition, leading to a misdiagnosis or a missed opportunity to seek sleep apnea treatment. For example, OSA patients may report symptoms of anxiety. Anxiety can result from many things – a psychological disorder, medications, or prolonged sleep deprivation.13
Furthermore, some report having heart arrhythmias while sleeping, as if their heart is skipping a beat or is racing. This can be a result of a cardiac problem or obstructive sleep apnea.14 Here is a short list, but be sure to read our comprehensive symptoms article at the end of this section.
- Loud and chronic snoring
- Choking, snorting, or gasping during sleep
- Lapses in breathing
- Waking up feeling short of breath
- Daytime sleepiness and fatigue
Lesser-known signs:
- Waking up with a dry mouth or sore throat
- Insomnia or nighttime awakenings
- Going to the bathroom frequently during the night
- Forgetfulness and difficulty concentrating
- Uncharacteristic moodiness, irritability, or depression
- Morning headaches
- Impotence
Both genders seek medical assistance for sleep apnea but reasons for seeking an initial consultation may differ. Men may seek treatment due symptoms of snoring, a disinterest in sex or erectile dysfunction,15 or even hair loss.16
Women may report symptoms of anxiety or depression. Sleep deprivation has a negative impact on the brain and its ability to replenish the body. The neurochemical deficiency often results in symptoms of anxiety and depression.17 While it’s a causal factor, ongoing anxiety leads to greater problems. Read more about major and minor symptoms, risk factors, and how to get a better night’s sleep.
Explore Sleep Apnea Symptoms
Associated Health Risks
Take your pick of an area of the body and you can trace an associated health risk to sleep apnea. As mentioned, sleep apnea is linked to depression.18 63% of those suffering from OSA also report symptoms of depression.19
Furthermore, people are at risk of heart disease when getting insufficient sleep. Poor sleep or rising too early can lead to increased inflammation, which underlies a link between poor sleep and cardiovascular disease. Poor sleep and increased risk of developing heart problems affect both sexes, but research has shown a few factors for heart disease are especially linked to women.20
OSA is also linked to elevated blood sugar levels.21 When the airway is partially or completely blocked the body tries to signal the brain that you aren’t sleeping (even though you are). This is so your airway will open up and let oxygen in. When you’re not getting enough air the diaphragm must work harder and your oxygen levels may drop or CO2 levels may go up in your blood which alerts the brain. When the brain senses the low oxygen or increased work of the diaphragm the brain registers that you’re airway is obstructed so and releases norepinephrine, which causes an arousal in your brainwaves (EEG) to make it more like you’re awake even though you’re not awake, brings the muscle tone back to the airway.
Norepinephrine is best known as a stress hormone and a main component of the fight or flight response. It also raises blood sugar. When you have untreated or undiagnosed obstructive sleep apnea, you’re releasing norepinephrine throughout the night in response to airway blockages, because the obstruction of airflow compromises the body’s oxygen. The end result of this cycle is higher blood sugar because the neurotransmitter is counterregulatory to insulin. Those with type 2 diabetes may have trouble controlling their condition due to an undiagnosed case of OSA.
Major health risks:
- Stroke
- Obesity
- Heart Disease
- Heart Attack/Heart Failure
- Hypertension
- Type 2 Diabetes
- Liver Problems
- Adult Asthma
Memory loss or “brain fog” can be a sign of many things, and it’s linked to sleep apnea. The body needs regular sleep to replenish itself. Disruptions in sleep patterns influence the production of certain types of neurochemicals, such as serotonin.22 Such neurochemicals help us plan, focus, and concentrate on cognitive functioning.
So, sleeping problems result in memory problems or brain fog. Actually, sleep deprived people make twice as many errors and are three times more likely to have lapses in attention.23 However, the good news is that once you address the sleep disorder, you can alleviate the memory issues.
Many health problems are related to sleep apnea. However, early detection means that a lot of minor to major repercussions are completely preventable. Learn more about health risks and how you can seek sleep apnea treatment.
Explore Sleep Apnea Health Risks
Sleep Apnea Diagnosis and Treatment
A sleep study is extremely important in diagnosing a sleep disorder and defining proper treatment. A polysomnogram is the most common diagnostic tool and is a comprehensive recording of physiological changes occurring during sleep. The study is conducted overnight at a sleep center, where a credentialed technologist monitors 14 separate channels including brain activity (EEG), heart rhythm (ECG), and eye movements (EOG), among others.
Whether you are researching on your own or your doctor suggested a sleep study, it is normal to be curious about how an in lab sleep study works and what to expect. To help you better understand sleep studies, we’ve created a detailed online guide that walks you through everything you need to know about a sleep study and what you can expect during your study if one is necessary. Our patients report feeling more knowledgeable, comfortable, and prepared after reading the guide; they also tell us they better understand how and where a sleep study fits on their personal journey to better sleep.
Explore Sleep Studies
In-Home Sleep Test
An in-home sleep test is a fast and cost-efficient way to confirm sleep apnea. There are different home sleep tests available. All sleep tests track breathing patterns and oxygen saturation levels, with more advanced testing equipment also collecting additional data such as heart rate, circadian rhythms, body position, and actual sleep time.
While home sleep tests are not as comprehensive as a sleep study performed at a sleep center, an in-home test can be a link between a common symptom, such as snoring or depression, and getting an official study performed at a sleep center.
Read More About In-Home Sleep Tests
CPAP Therapy
CPAP therapy is one of the most common treatments for sleep apnea. CPAP is the safest, least expensive, and most efficient way to treat obstructive sleep apnea. CPAP (or continuous positive airway pressure) provides enough pressure to keep the airway clear of obstruction. In simple terms, OSA is just a blocked airway and CPAP therapy unblocks it.
Everyone has questions about CPAP that range from how it makes you feel after you use it to how it feels to wear a device while you sleep. Probably the most common is, will it disturb my sleep? Will I be equally unrested because I’m wearing a CPAP (the short answer is no, you adapt very quickly, especially because you are not being awoken by hypopneas and apneas)?
Explore CPAP Therapy
CPAP Machine
A CPAP machine is a piece of durable medical equipment that delivers continuous positive airway pressure through a small mask or nasal pillows as you sleep. The CPAP machine helps maintain open airways while you sleep, significantly reducing hypopneas and apneas allowing you to sleep peacefully and rest fully.
Like most medical devices, technology and manufacturing advancements have positively affected the size of the CPAP machine, the sound they make, as well as their ability to automatically detect and deliver the precise amount of pressure for you at exactly the right time throughout the night. Modern CPAP is a far cry from your grandparent’s noisy, cumbersome sleep machines!
Explore modern CPAP Machines and Supplies
Other Forms of Sleep Therapy
Oral Appliances Devices
Oral appliances help address obstructive sleep apnea. MADs or mandibular advancement devices and Tongue Retaining Mouthpieces push the tongue away from the back of the throat to prevent blockage.
Surgery
In rare cases, obstructive sleep apnea is treated with surgery to the areas of the throat, nose, or tongue. UPP (uvulopalatopharyngoplasty), the most common procedure, removes excessive tissue.
Read more on Sleep Apnea Treatments
What is sleep apnea?
Sleep apnea is a common sleep disorder characterized by interruptions in normal breathing. During sleep, the throat muscles relax, and the air passage becomes obstructed by the soft tissue in the mouth and throat.
What are the common sleep apnea symptoms?
Common symptoms of sleep apnea include snoring, daytime drowsiness, morning anxiety and depression, waking up with a sore throat and/or headache, brain fog, forgetfulness, lack of interest in sex and moodiness. Anyone experiencing two or more of these symptoms should consult a doctor.
What are the associated health risks of sleep apnea?
Sleep apnea is unlikely to be the direct result of death. However, left untreated sleep apnea can lead to or worsen dangerous health problems like heart disease, stroke, type 2 diabetes, adult asthma, heart attack, high blood pressure, obesity and liver problems.
How do I test and diagnose sleep apnea?
Sleep apnea is diagnosed through a sleep study known as a polysomnography which measures heart rate, blood-oxygen levels, brain waves, breathing as well as eye and leg movements. Additionally, there are home testing kits for sleep apnea which are often used to determine if a polysomnography is necessary.
Are there any sleep apnea treatments?
Continuous positive airway pressure or CPAP is the most common and most effective method of treating sleep apnea. However, there are other potent treatments like positional therapy, adjustable oral appliances, surgery and lifestyle changes.
What do I need to know about CPAP?
A (Continuous positive airway pressure) CPAP device is worn on the face during sleep and supplies air pressure to the breathing passage to keep it free from obstruction. It is highly effective at treating sleep apnea if worn consistently. To be sure, there are a variety of models available to ensure a good fit and performance.
- https://www.hopkinsmedicine.org/health/wellness-and-prevention/the-dangers-of-uncontrolled-sleep-apnea
- https://www.webmd.com/sleep-disorders/sleep-apnea/features/sleep-apnea-clues
- https://www.medicalnewstoday.com/articles/319378
- https://sleepmeeting.org/wp-content/uploads/2019/04/SLEEP_42_S1-Website-Final.pdf
- https://aasm.org/resources/pdf/sleep-apnea-economic-crisis.pdf
- https://pubmed.ncbi.nlm.nih.gov/23589584/
- https://healthblog.uofmhealth.org/health-management/10-alternatives-to-cpap-for-treating-obstructive-sleep-apnea
- https://healthblog.uofmhealth.org/health-management/10-alternatives-to-cpap-for-treating-obstructive-sleep-apnea
- https://www.mayoclinic.org/diseases-conditions/central-sleep-apnea/symptoms-causes/syc-20352109
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5443744/
- https://www.sciencedaily.com/releases/2006/09/060901161349.htm
- https://www.sciencedaily.com/releases/2018/10/181019131518.htm
- https://sleepcenterinfo.com/blog/sleep-deprivation-effects-on-brain/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2841803/
- https://sleepcenterinfo.com/blog/sleep-deprivation-and-erectile-dysfunction/
- https://sleepcenterinfo.com/blog/can-sleep-apnea-cause-hair-loss/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181635/
- https://sleepcenterinfo.com/blog/heres-how-your-cpap-machine-can-decrease-depression/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3296787/
- https://pubmed.ncbi.nlm.nih.gov/23746737/
- https://spectrum.diabetesjournals.org/content/29/1/14
- https://brainmd.com/blog/serotonin-can-help-with-sleep/
- https://psycnet.apa.org/buy/2019-70149-001