About 70 million American adults experience chronic sleep problems and poor sleep each year. Common sleep problems include serious sleep disorders like obstructive sleep apnea (OSA) and insomnia.
Obstructive sleep apnea (OSA), often identified by the sound of snoring, is when the airway is either partially blocked or in rare instances completely obstructed. This obstruction makes it difficult to breathe when sleeping, and contributes to serious disease states and health risk factors.
Insomnia, either acute or chronic, means you’re struggling to fall asleep or having difficulty staying asleep or going back to sleep if you wake up in the night.
Having either sleep disorder individually is difficult, but having both insomnia and sleep apnea can have serious effects on your sleep health, and overall health. It can be a very dangerous— and potentially deadly— combination.
Proper treatment is the key, no matter how many sleep disorders you may have.
A sleep professional can help you treat multiple sleep disorders. They can also discuss the connection between sleep apnea and insomnia, and how best to approach your treatment.
Is There a Connection Between Sleep Apnea and Insomnia?
While the two sleep disorders are very different, there is a connection between obstructive sleep apnea and insomnia. In fact, 50 to 60 percent of people who have been diagnosed with one sleep disorder likely have the other as well.
Insomnia and obstructive sleep apnea (OSA) are so closely connected that there’s even a term for having both— comorbid insomnia and obstructive sleep apnea, or COMISA.
According to the European Respiratory Review, it can be difficult to determine the relationship between obstructive sleep apnea and insomnia in individual patients. This may happen for three reasons:
- One disorder could be a side effect or symptom of the other
- The two disorders could be negatively impacting each other and aggravate each other’s symptoms
- The conditions may occur unrelated to one another
For example, if you have OSA and experience multiple respiratory events each night you may develop insomnia as a result of your breathing interruptions.
Conversely, an insomniac with a low respiratory arousal threshold— meaning they are less likely to wake up if they experience sleep-disordered breathing— may be more likely to have obstructive sleep apnea. In fact, the European Respiratory Review observed this trait in 37 percent of COMISA cases during their study.
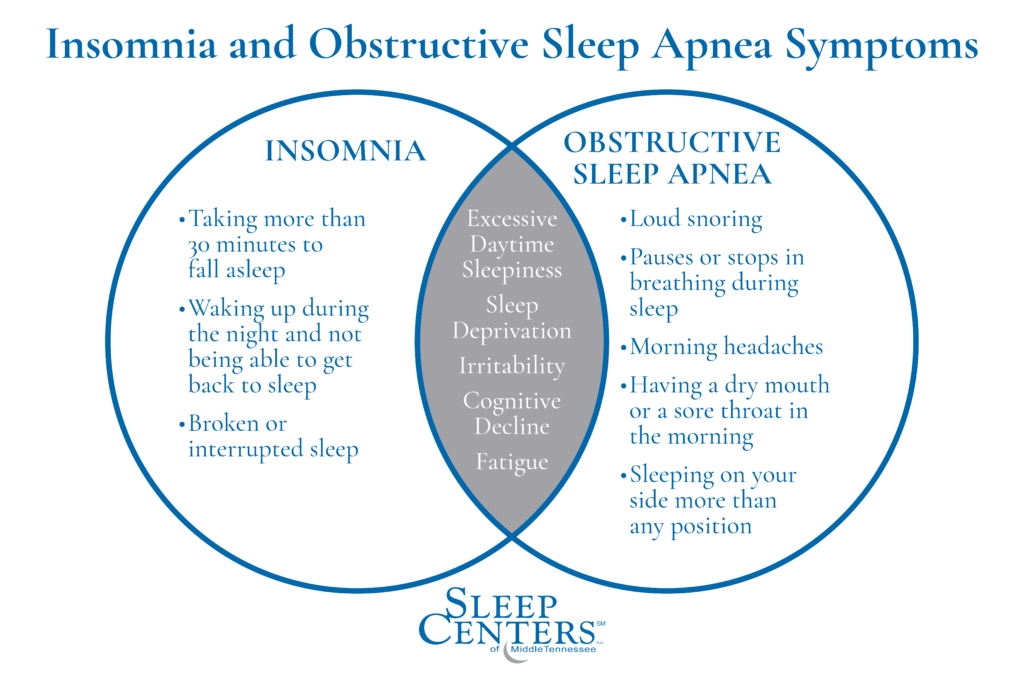
To make matters more complex, both sleep disorders share common symptoms, making it more difficult for you to determine which one may be affecting you. Some of these commonalities may include:
- Excessive daytime sleepiness
- Sleep deprivation
- Irritability
- Cognitive decline
- Not feeling rested even after a full night’s sleep
While you may feel some of these symptoms in as little as one night of poor sleep, these symptoms are more commonly experienced in the long term. And if you have been experiencing these symptoms for a while, then that’s a sign that something is definitely wrong.
Sleep Apnea and Insomnia: A Potentially Deadly Combination
A recent study from Flinders University found that people who have both obstructive sleep apnea and insomnia are at increased risk of increased blood pressure, heart disease, and even premature death. Even more concerning, if you have both sleep disorders, there’s a 50 percent higher likelihood of dying for any reason, compared to people with only one or neither disorder.
This study’s findings were reported after observing over 5000 participants around 60 years old over approximately 15 years.
Researchers observed that patients with COMISA (having both sleep apnea and insomnia) are:
- Twice as likely to have high blood pressure than those without sleep apnea or insomnia.
- Seventy percent more likely to have cardiovascular disease than those who did not have either sleep disorder.
- At a 47 percent higher risk of mortality than those without either condition, even after considering other factors that could increase their mortality rates.
Note: 1210 participants passed away over the course of the study— the study did not disclose how many passed from heart disease, or as a direct result of COMISA.
Although the associated health risks that OSA and insomnia can have on your health are well documented, more research is needed to determine the exact cause of COMISA’s increased mortality risk. Because of this, researchers encourage OSA patients to get tested for insomnia, and insomnia patients to get tested for OSA.
But oftentimes it’s much easier said than done to know and understand your symptoms so you can get tested.
COMISA Diagnosis and Treatment
Patients suffering from COMISA can blur the line between the two disorders making it more difficult to diagnose and treat properly.
When both sleep disorders are diagnosed, you may need more specific treatment to adequately address the effects of both. This treatment may include additional monitoring to ensure effective treatment and safe integrations of medication if multiple are necessary.
Treatment for both disorders is vital though, not just for your sleep but for your overall health too.
How to Get Started
You can take our sleep apnea quiz to uncover whether your symptoms indicate you’re at risk for obstructive sleep apnea. Then talk to your doctor or a sleep specialist about whether sleep apnea is contributing to your insomnia or whether insomnia is a sign you may have undiagnosed sleep apnea.
A sleep specialist can help evaluate your symptoms and decide whether a sleep study is needed to determine the cause of your sleep problems. You can reach out to us for an evaluation if you live in the Nashville, Murfreesboro, Cool Springs or Clarksville, Tennessee areas.
In the meantime, there are steps you can take to get better sleep while waiting for a possible diagnosis.
Related: Can You Die from Insomnia?
How to Get Better Sleep If You Have Sleep Apnea and Insomnia
Taking steps to get healthy sleep overall is important— especially when suffering from more serious sleep disorders like sleep apnea and insomnia.
Here are our four tips for getting better sleep:
1. Follow a Consistent Bedtime Routine
Consistency is key!
A consistent bedtime routine can help your body prepare itself for a good night’s sleep. By going to bed at the same time every night and waking up at the same time each day, your body creates a schedule. Once your body is used to this schedule, it can more easily prepare itself to be asleep or awake at your desired times.
This is especially important if you have a sleep disorder because this consistency can make a huge difference in your overall sleep quality.
What you do before bed matters too.
For better sleep, we recommend dedicating the last hour before bedtime to winding down and wrapping up any unfinished tasks. Getting your body and brain relaxed and at ease before bed is essential.
You might spend the last hour before bed taking care of your pets or getting your kids ready for bed. Then take care of personal hygiene before settling down to do something relaxing like reading a book, meditating, or writing in a sleep journal.
To ensure a good night’s sleep avoid activities that may raise your heart rate prior to your desired bedtime, like working out.
Additionally, you should avoid using electronic devices prior to bed. Phones, tablets, and desktops emit blue light that can hinder your body’s natural melatonin production, making it harder for you to fall asleep and stay asleep.
2. Avoid Large Meals, Caffeine, and Alcohol Before Bed
Consuming large meals, drinking caffeine after approximately 2 PM, or drinking too much alcohol within a couple of hours before going to bed will disrupt your sleep.
Here’s why:
Your body will prioritize digestion over falling asleep when you consume a large meal too close to bedtime. Your body is hard at work digesting your food rather than helping you fall asleep!
Large meals can also contribute to poor sleep by increasing your risk of heartburn or acid reflux.
To avoid heartburn or reflux, it’s best to stop eating at least a few hours before your regular bedtime. This gives your body plenty of time to digest your food and reduce your risk of heartburn or reflux.
Caffeine’s stimulant effects are well-known, and consuming caffeine too close to your normal bedtime can keep you awake, and ruin your sleep (even if you are able to fall asleep).
To prevent sleep disruption, stop consuming caffeine 6 to 8 hours before your bedtime to reduce the caffeine in your system by the time your head hits the pillow.
If you enjoy a nightcap before bed or even a few cocktails during supper, when you take your last sip is important where sleep is concerned. It’s generally recommended that your last drink should be 3 hours before bed.
Ironically, many people drink alcohol close to bed believing it’s a sleep aid, but alcohol does more harm than good for restful sleep.
Alcohol can lead to increased sleep disturbance at night, can trigger nighttime heartburn, and can worsen sleep-disordered breathing. This includes regular snoring, as well as obstructive sleep apnea. It can also reduce the amount of REM sleep you get each night.
Related: Alcohol and Sleep May Not Mix as Well as You Think
3. If You Already Have Insomnia or Sleep Apnea, Get Tested for the Other Sleep Disorders
In addition to the findings above, the researchers involved in the Flinders University study also note the importance of getting tested for both insomnia and obstructive sleep apnea, especially if you already have one of the conditions. This is an important step to understanding your sleep needs and how it’s impacting your overall health.
Without realizing it, your undiagnosed sleep apnea or insomnia can be a major factor in your health and potential health issues. You, like many others, may not know you have a sleep disorder. This is common because many of the symptoms occur while sleeping, or your symptoms are being attributed to something else.
Undiagnosed sleep disorders can also make treatment for other health problems less effective because they don’t address the problems caused by the sleep disorders themselves.
This is why it’s so important for you or your sleep partner to be aware of symptoms of sleep disorders like OSA or insomnia. Some insomnia symptoms to be aware of include:
- Difficulty falling asleep
- Waking up during the night, or waking up too early in the morning
- Continuous worries about sleep, which can also keep you up at night
Sleep apnea symptoms to know include:
- Pauses in breathing while you sleep
- Coughing, choking, or gasping for air during the night
- Extremely loud, persistent snoring
Remember— sleep apnea and insomnia often share the same symptoms, making them difficult to diagnose on your own. That’s why you should be tested for both sleep disorders if you already have one or the other.
If you’re at risk for sleep apnea, get an evaluation for a sleep study to determine whether a home sleep apnea test or an in-lab sleep study is needed.
For many, home sleep test results will be enough to diagnose sleep apnea. For others, an in-lab sleep study is required. This may be especially true for someone suffering from both insomnia and obstructive sleep apnea.
Sleep studies involve overnight testing that monitors your breathing, brain activity, and muscle activity to identify abnormalities that are harming your sleep.
4. Follow Your Prescribed Sleep Disorder Treatments
Remember, sleep disorders require the correct treatment in order to improve your symptoms in the long term. So if you’re being treated for one or multiple sleep disorders, be sure to follow all your doctor’s instructions. Remember— consistency is key!
Common treatments for insomnia symptoms include prescription or over-the-counter sleep aids, or cognitive behavioral therapy.
The most common treatment for obstructive sleep apnea is CPAP therapy. CPAP— continuous positive airway pressure— is highly effective, but many patients may struggle to stick to their treatment because they find the apparatus bulky, uncomfortable, or maybe even ineffective.
If you think your prescribed treatment may be ineffective, talk to your doctor or a sleep specialist. They can help you find alternative treatments for your sleep disorder symptoms. Never stop or alter your treatment without your doctor’s permission.
You should never ignore any sleep problems you may be experiencing. Not only can untreated sleep apnea or insomnia ruin your sleep, but they can put your overall health in danger too.
If you’re not sure if you have a sleep disorder, a good night’s sleep may just be a sleep study away. Contact us at the Sleep Centers of Middle Tennessee today! We can help you schedule an evaluation of your symptoms and start getting back to the healthy sleep you need to be at your best.
References
Janssen, Hennie C.J.P., et al. “Management of Insomnia in Sleep Disordered Breathing.” European Respiratory Society, European Respiratory Society, 30 Sept. 2019, err.ersjournals.com/content/28/153/190080.
“Common Sleep Disorder Combo Could Be Deadly.” ScienceDaily, ScienceDaily, 13 Dec. 2021, www.sciencedaily.com/releases/2021/12/211213121813.htm.