
Untreated OSA has a High Mortality and High Prevalence
Obstructive sleep apnea (OSA) is present by the most recent data (Malhotra, AASM abstract June 2019) in 37% of adult Americans with roughly half of those having moderate or severe OSA, and 80% of cases are undiagnosed.
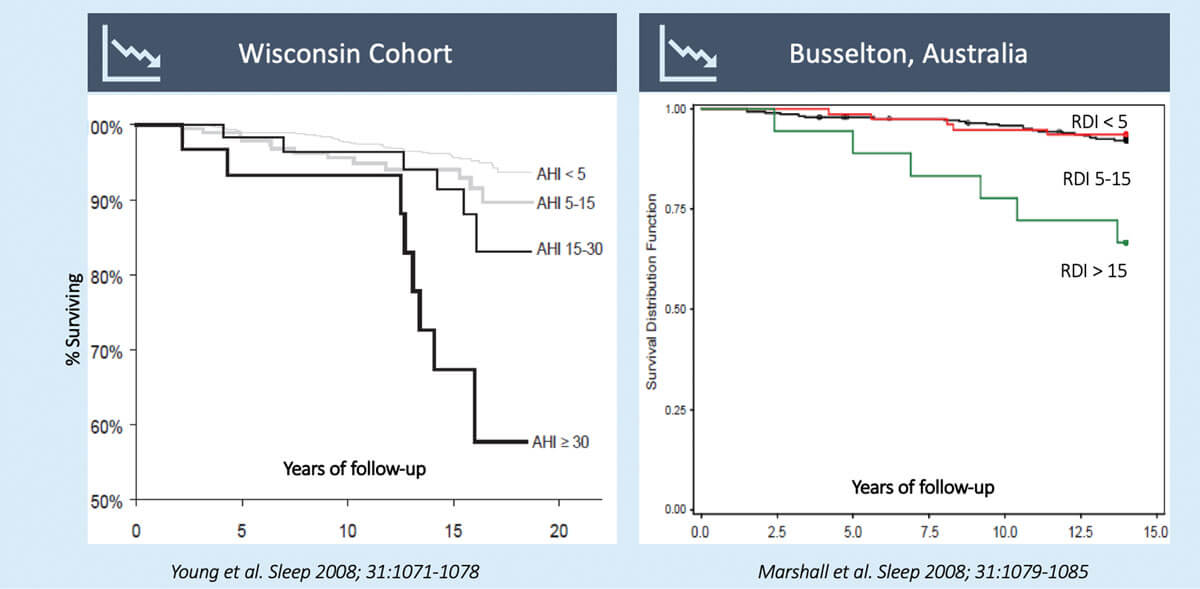
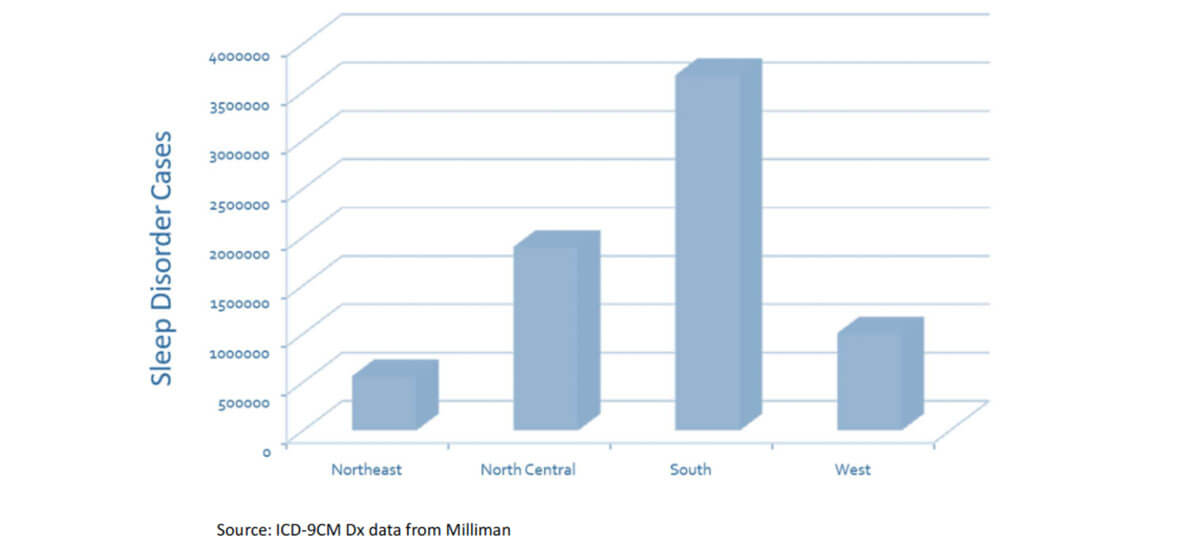
Untreated moderate and severe OSA have marked increased mortality as high as 40% over 12-15 years. Roughly 1 in 5 adults have this increased mortality, which is likely more prevalent in the southeast US where obesity rates are highest.
Consequences of not Treating Mortality
Prevalence of OSA in the US by Region
While OSA is highly prevalent in the general adult population, OSA is even more prevalent in the waiting rooms of primary care providers. This is because waiting rooms usually have patients with disease where OSA is highly prevalent, and often causative.
Prevalence of OSA in Outpatient Clinic
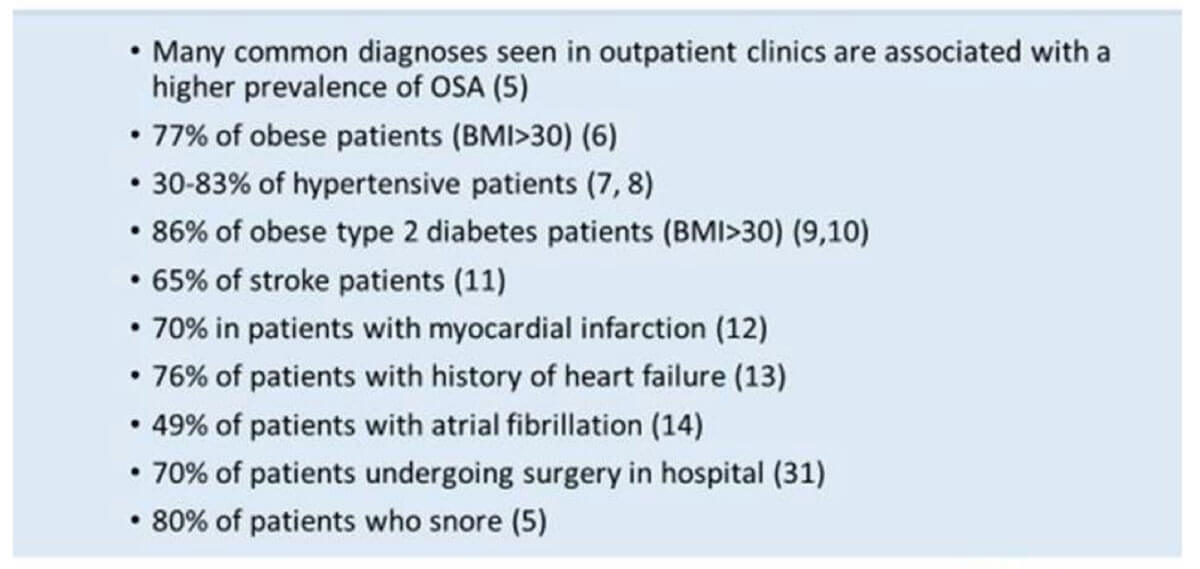
Providers who specialize in adult diabetes likely have an 80% prevalence of OSA in their waiting room, and many of these patients would immediately improve their blood sugar control with treatment of OSA.
OSA is also highly prevalent in patients with cardiovascular disease, possibly as high as 70%. Yet, Costa et. al found (Heart 2015) only a small percentage of patients with CVD undergo evaluations for OSA. With the strong evidence that “wearing” CPAP reduces cardiovascular events, this is disappointing. However, this small referral percentage may reflect more on the previous inconvenience, cost, and time required for sleep studies, and the historically poor adherence to CPAP, more than referring providers.
OSAinHomeSM removes many of the previous barriers to treatment.
Why is CPAP the Most Common Treatment?
OSAinHomeSM is a program for patients at risk for sleep-disordered breathing (SDB) of which obstructive sleep apnea (OSA) is the most common type. Continuous positive airway pressure (CPAP) is by far the most common treatment prescribed by sleep medicine physicians to treat OSA for five main reasons:
CPAP is by far the safest therapy. Though sometimes inconvenient, CPAP has very limited side effects for which there are easy solutions. Other treatments can have serious side effects. There have been deaths after surgery for OSA. Even oral appliances can move teeth and cause severe cases of TMJ disease, especially when used in moderate to severe cases.
CPAP is the most cost-efficient treatment. CPAP is ½ to ¼ of the cost of an oral appliance, and surgery can be 50 times the cost of CPAP. There is substantial evidence that CPAP saves downstream healthcare costs as well. There is none with other treatments.
There is strong evidence that CPAP reduces cardiovascular (CV) events, hospital readmissions, etc. and improves blood pressure, blood sugar control, cognitive function, mood disorders, quality of life (QOL), etc. There is little evidence with other treatments. Therefore, CPAP should be recommended first for even mild OSA in patients with cardiovascular disease.
Contact Us for Info or Send Patients for OSAinHomeSM
OSAinHomeSM Provides Your Patients 44% Higher CPAP Adherence
That means less risk of Cardiovascular Events and less healthcare costs
In order to gain the benefits of CPAP patients must wear CPAP consistently through the night. If a patient fails to wear CPAP consistently and long-term, the efforts in diagnosis and treatment were a waste of time and money.
Historically, adherence to CPAP has been poor as has been evident in many randomized clinical trials (RCT). The largest RCT for prevention of CV events (SAVE study, NEJM September 2018) had only 42% of participants in the treatment group still using CPAP at one year despite removing 15% of non-adherent participants before randomization, meaning only 27% overall were still using CPAP at one year.
This poor adherence is why many RCTs initially fail to show reduction in CV events. Secondary analysis of the SAVE study as well as other RCTs (looking at those participants who used CPAP long-term), and observational data shows CPAP reduces CV events, but then this data is no longer randomized.
Across the literature, average CPAP usage > 4hrs/night over one year generally produces outcomes, like reduction in CV events; average usage < 4hrs/night over one year generally does not produce outcomes (exceptions include HTN, Insulin resistance, excessive sleepiness, QOL, and MVAs). This is true for a population. For an individual it appears 6hrs/night is required.
CPAP Reduces Cardiovascular Events
12 year study shows incidence of cardiac events in untreated vs. CPAP patients with OSA
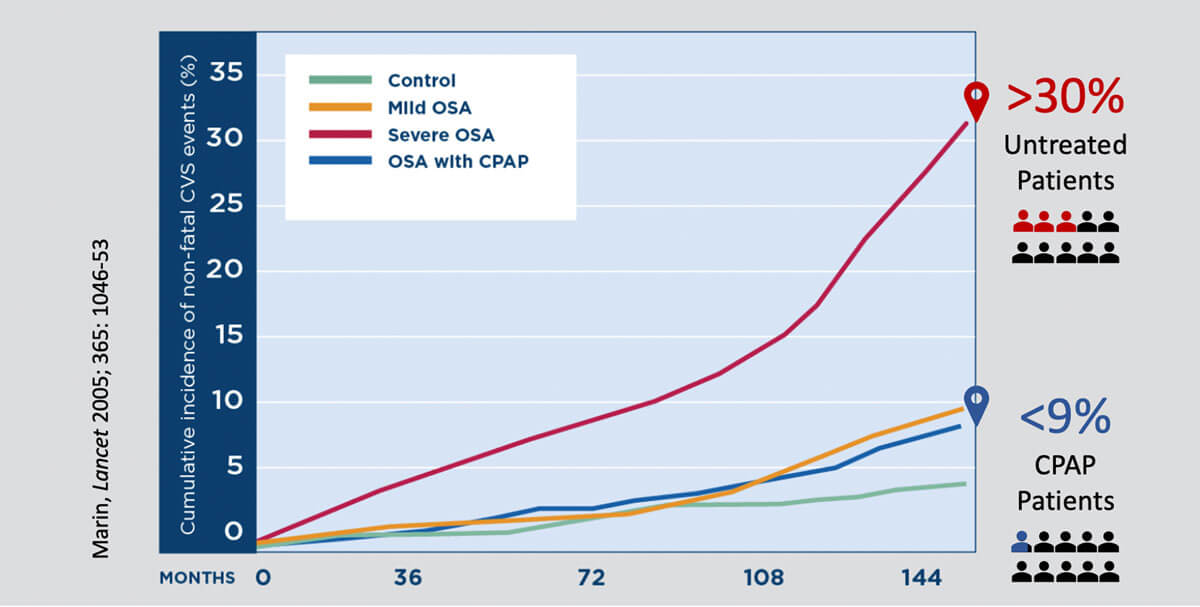
Non-randomized data can have confounding factors. For example, someone who chose to wear CPAP may have also exercised more or had a healthier diet. But it is clear that “wearing CPAP” reduces CV events. Poor adherence in RCTs prevents us from saying that the CPAP machine itself prevents CV events. Yet, if “wearing CPAP” reduced CV events by two-thirds over 12 years (like the Marin study above), and the cost of a revascularization is 50-100 times the cost of CPAP, then a payor should want to identify and treat all moderate and severe cases. Again, this would be dependent on adherence.
The improvement from CPAP was so significant in some RCTs that despite poor adherence (< 4hrs/night) the trials still showed improvement in hypertension, insulin resistance, QOL, and daytime sleepiness, as well as reduction in motor vehicle accidents (MVA). For more detailed explanation of RCTs and CV events and the references referred to above, please see the editorial by OSAinHomeSM Medical Director.
Read editorial: “Using CPAP” Improves Cardiovascular Outcomes: Physicians must look behind the RCT veil and focus on long-term adherence
Outcomes for OSA are dependent on CPAP adherence. For a population of patients, twice the adherence should produce twice the outcomes of improvement, and therefore, OSAinHomeSM measures its quality of care by CPAP adherence.
Read Google Reviews from Sleep Center of Middle Tennessee’s Patients >
Contact Us for Info or Send Patients for OSAinHomeSM
OSAinHomeSM’s Higher CPAP Adherence
SCMT was the first to use social cognitive theory to provide OSA education to improve CPAP adherence across a whole practice. Beginning in 2007, all of our clinical staff who interact with patients and provide OSA education were trained in processes like motivational interviewing and cognitive behavioral therapy to improve adherence to CPAP.
See our staff training protocol >
Combining remote monitoring with trouble shooting, CPAP education, and behavioral intervention, SCMT created DREAM (Directed Remote Education and Adherence Monitoring) more than a decade ago.
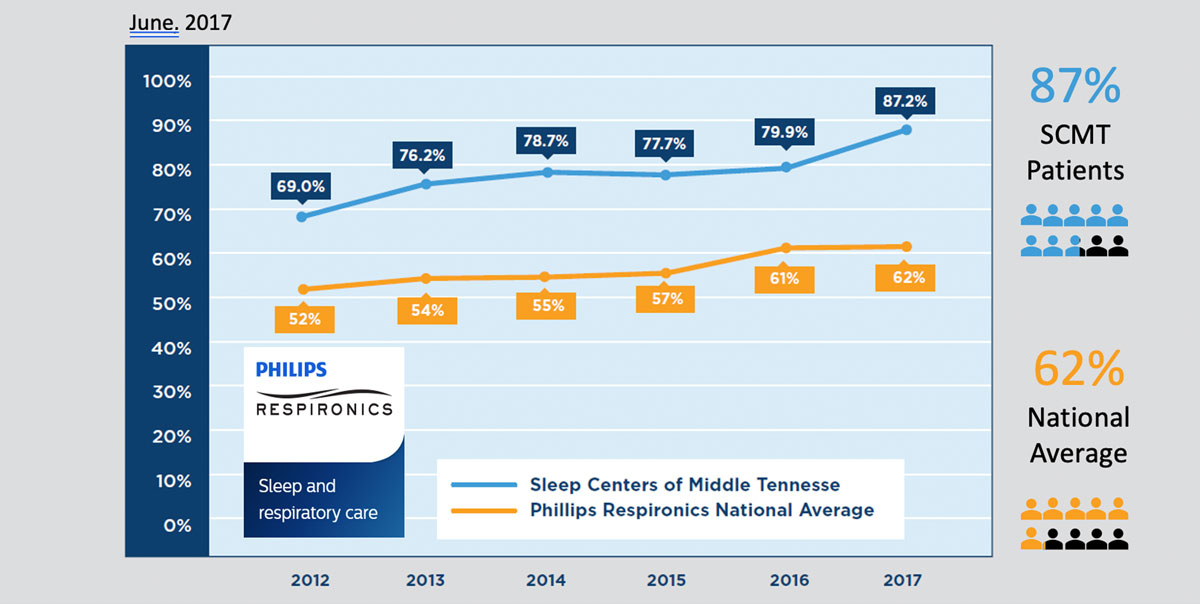
So, what are the results? SCMT’s DREAM Program maintained 32-44% increase in CPAP adherence over the national average from 2012-2017 (data supplied by manufacturer database with 6.8 million patients).
CPAP Compliance Among SCMT Patients vs. National Average
7,657 SCMT Patients | 6.8M Phillps Respironics Patients
By 2017 DREAM had collected CPAP adherence data on nearly 16,000 consecutive patients and SCMT partnered with Middle Tennessee State University (MTSU) to form the MTSU Sleep Research Consortium. MTSU faculty and graduate students began to analyze DREAM CPAP adherence data.
Patients dispensed CPAP through an integrated sleep medicine physician practice have much greater long-term adherence than patients dispensed CPAP through the traditional medical equipment company model.
SCMT CPAP Usage Obtains Outcomes
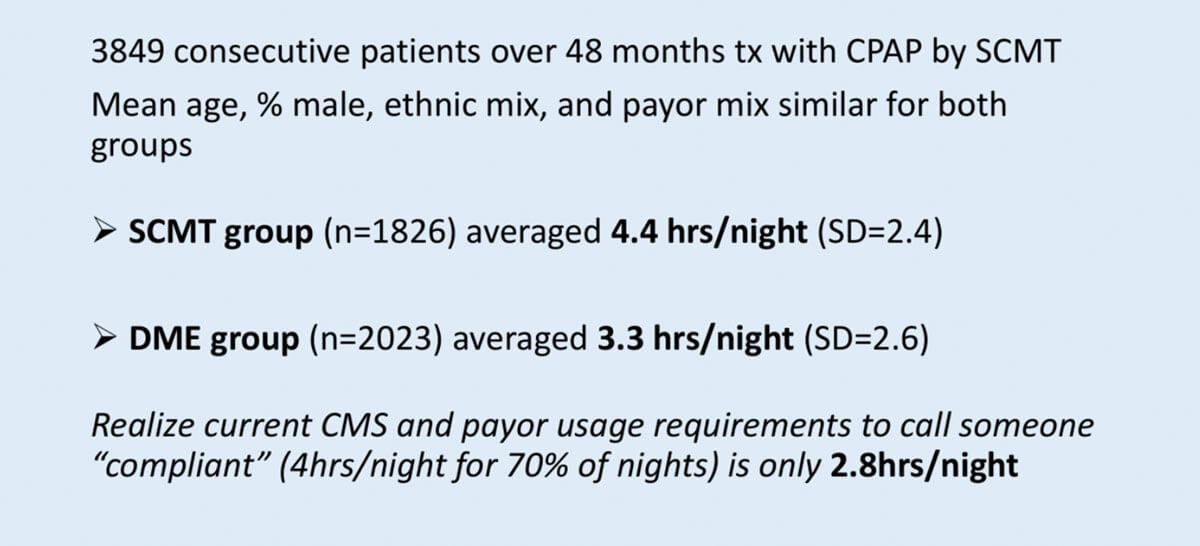
The above data (manuscript submitted) reveals that there were two levels of care within SCMT: Those provided CPAP by SCMT with DREAM, and those provided CPAP by a DME company.
Both groups had the same medical care by the same providers using the same protocols and had their studies in the same facilities.
The SCMT group far exceeds the usage to reduce CV events; the DME group, though with usage above the national averages, would not reduce CV events.
Notice the CMS requirement (used by many commercial payors) is far below the level to reduce CV events. Payors like BlueCross BlueShield, Anthem, Aetna, United Health Care, etc. who allow their members to obtain their CPAP from SCMT are likely having greater QOL, better blood pressure and blood sugar control, and fewer MVAs and CV events.
Introducing DREAM 2.0: Monitoring New CPAP Patients for 7 Months
For years we remotely monitored and intervened with non-adherent patients for 3 months, assuming that once they were averaging at least 6 hours/night that they would continue to use CPAP long term. We found it actually takes 7 months to determine long term usage, and this 7-months point is true regardless of age, sex, race, or source of CPAP.
12 Month Usage
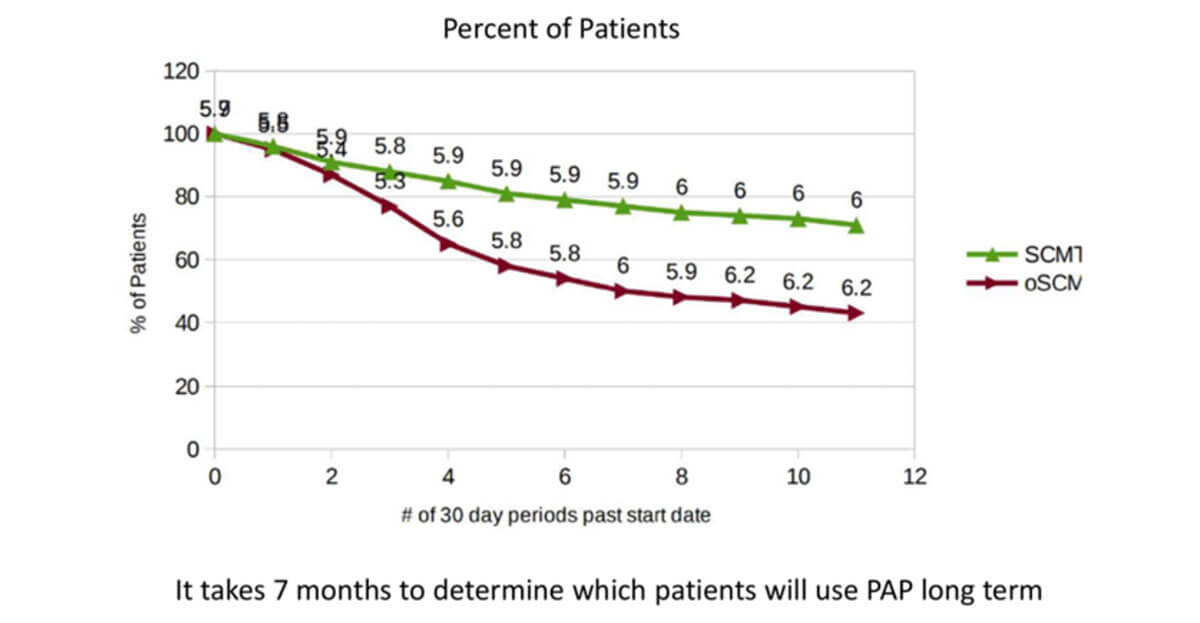
The green line in the above chart represents 1826 patients provided CPAP by SCMT from 2012-2016. The burgundy line represents 2023 patients treated by SCMT but provided CPAP by an outside DME company from 2012-2016. In both groups those using are averaging close to 6hrs/night; it is just the DME-supplied group (burgundy line) had more patients discontinue CPAP. Both groups were followed for only 3 months if they were averaging > 6hrs/night, which is clearly an inadequate length of time.
48 Month Usage
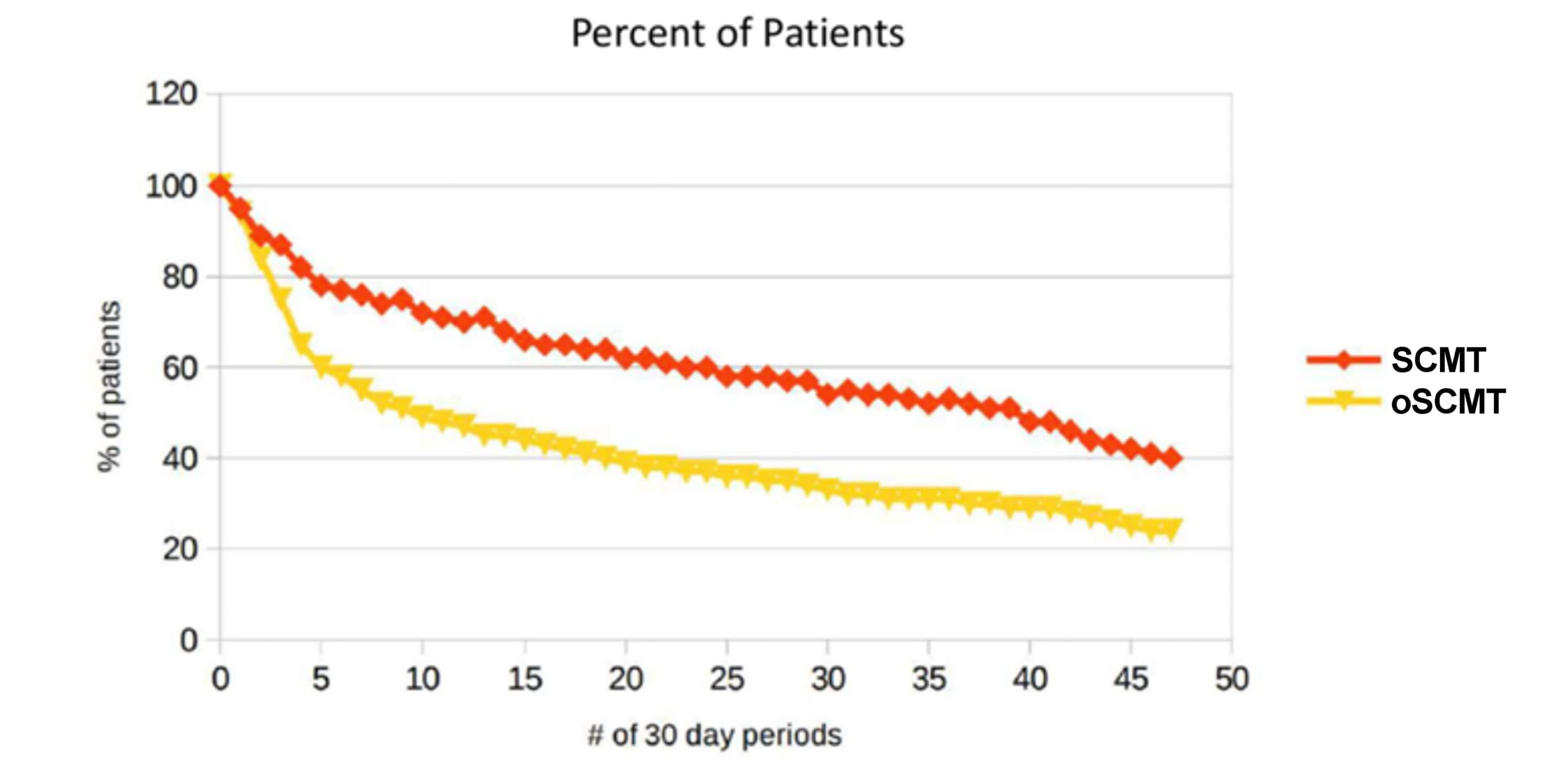
The red line in the chart above represents those provided CPAP by SCMT in 2012 and the yellow line represents those treated by SCMT but provided CPAP by a DME company. Notice again that the lines develop a constant slope after 7 months which represents an expected attrition and continues for 4 years.
It is interesting that the majority of patients who became non-adherent did so between months 3 and 7. We have subsequently reviewed the large Philips CPAP adherence database (>7 million) and found the same 7-month phenomenon. The SAVE study data appears to show a similar trend.
Philips recently published an abstract (AASM annual meeting, June 2019) showing increased adherence with remote monitoring and intervention with sleep coaches/respiratory therapists up to one year. Again, their adherence rates had no change after 7 months, but it strongly suggests that by OSAinHomeSM increasing adherence monitoring and intervention from 3 months to 7 months (DREAM 2.0), our percentage of users at 1 year could approach 90%. It will require a year for us to have data.
In summary, SCMT, and thus OSAinHomeSM, historically has long-term CPAP adherence rates (third-party verified) that are twice the average found in manufacturers databanks, and twice that found in RCTs. For a population of patients, one should expect twice the improvement in OSAinHomeSM patients. One cannot define quality of care any clearer. OSAinHomeSM is the only fully integrated OSA program in Tennessee. There are many home sleep testing companies, DME companies, sleep labs, and sleep providers which together provide a fragmented and often confusing front to patients. This is likely part of the explanation for OSAinHomeSM’s better outcomes. Don’t your patients deserve OSAinHomeSM’s speed to treatment, convenience, cost-savings, and most importantly, higher CPAP adherence?
Contact Us for Info or Send Patients for OSAinHomeSM
OSAinHomeSM Provides the Most Cost-Efficient OSA Care
When considering costs in treating OSA there are two types of costs:
Direct costs: Cost of office visits, sleep testing, and treatment (CPAP, oral appliances, and sleep surgery).
Indirect costs: Cost of increased medical care required by non-adherent CPAP patients.
OSAinHomeSM has the Lowest Combined Direct Costs
OSAinHomeSM Reduces the Most Indirect Costs
While it is difficult to quantify the indirect cost savings with CPAP, a recent large study throughout the Australian Health System (Streatfield, Oxford Univ Press, August 2019) found that treatment with CPAP > -$10,000 per DALY (Disability Adjusted Life Year). In other words, it is not only the extended life without disability that CPAP provides, it was actually less cost to treat OSA than to pay for the future cost of care associated with not treating the OSA. The adherence rate in the study was 57% which was higher than most RCTs, still below the long-term adherence of OSAinHomeSM. In the bar graph below, you can see how increased adherence decreases the indirect costs associated with OSA.
The medical literature clearly reveals cost saving with CPAP dating as far back as the 1990’s from the Canadian Health System and most recently from the Australian Health System (2019). In 2018, the Veterans Administration showed that CPAP reduced hospital readmission rates by 3 ½ times. There is a large cost reduction that CPAP provides in a population, and the point of the bar graph above is that this cost reduction is dependent on adherence. With 0% long-term adherence to CPAP (no one wearing long-term) a payor assumes 100% of the costs that could have been avoided. With 40% long-term adherence to CPAP (which is above the industry average) a payor mitigates 40% of the costs leaving 60%. Yet, with 80% long-term adherence a payor mitigates 80% of costs leaving 20% which is a 2/3 reduction in cost over the 40% adherence rate.
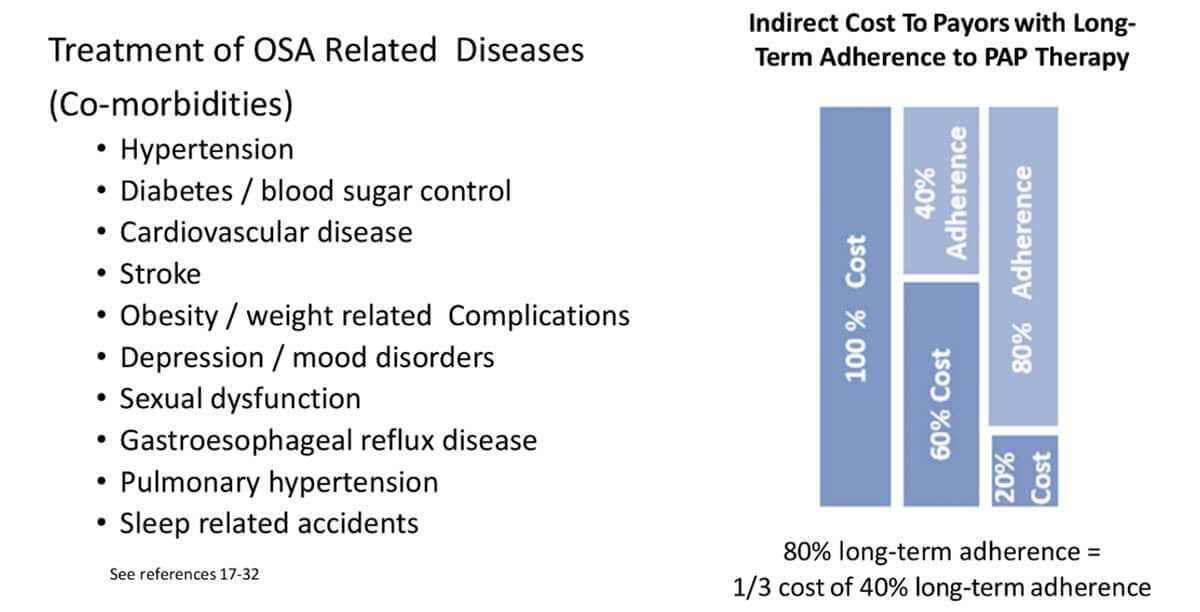
OSAinHomeSM long-term adherence rate may be reducing the indirect costs from OSA-related diseases by as much as 67% more than other sleep medicine providers in your network.